For decades, options for slowing the progression of chronic kidney disease (CKD) have been limited. Today, that’s changing. A new class of medications—SGLT-2 inhibitors—is transforming kidney and cardiovascular care, offering hope and protection for patients at risk of kidney failure and heart disease.
What Are SGLT-2 Inhibitors?
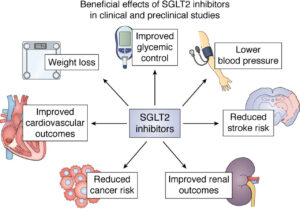
SGLT-2 inhibitors (Sodium-Glucose Co-Transporter 2 inhibitors) are a class of oral medications originally developed to lower blood sugar in people with type 2 diabetes. They work by preventing glucose reabsorption in the kidneys, causing excess sugar to be excreted in the urine.
But their benefits go far beyond glucose control. Clinical studies have shown that SGLT-2 inhibitors protect kidney function, reduce proteinuria, and significantly lower the risk of heart failure and cardiovascular death—even in patients without diabetes.
Why This Matters to patients with CKD
SGLT-2 inhibitors are the first class of drugs in decades shown to slow the progression of CKD across a wide range of patients. At Connecticut Kidney and Hypertension Specialists, we’ve embraced this therapy as a breakthrough, because for years, nephrologists had no truly disease-modifying treatments for most CKD patients beyond blood pressure and glucose control.
“This is one of the most exciting advances in kidney care in years,” says Dr. Ciampi nephrologist at Connecticut Kidney and Hypertension Specialists. “We now have a tool that not only protects kidney function but also helps prevent heart failure and death… new medications we are excited to offer our patients to slow down chronic kidney disease and help patients live longer and healthier free from from dialysis .”
Early Impact: The Evidence Is Strong
-
DAPA-CKD Trial: Dapagliflozin reduced the risk of CKD progression or death from kidney/cardiovascular causes by 39% in both diabetic and non-diabetic patients.
-
EMPA-KIDNEY Trial: Empagliflozin reduced the risk of disease progression or death from cardiovascular causes by 28%.
-
Number Needed to Treat (NNT): As low as 19–24 to prevent one major renal or cardiovascular event over ~2 years.
-
Early Benefits: Within 6–12 months, studies show significant slowing in eGFR decline, reduced proteinuria, and fewer hospitalizations for heart failure.
Who Should Consider SGLT-2 Therapy?
We recommend discussing SGLT-2 inhibitors if you have:
-
-
CKD with eGFR ≥ 20–25 mL/min/1.73 m², especially with proteinuria (UACR ≥ 200–300 mg/g).
-
-
Type 2 diabetes with CKD or cardiovascular disease.
-
A history of heart failure or at high risk of cardiovascular events.
Common medications in this class include:
-
Dapagliflozin (Farxiga®)
-
Empagliflozin (Jardiance®)
-
Canagliflozin (Invokana®)
-
Ertugliflozin (Steglatro®)
Monitoring and Sick Day Protocol
While SGLT-2 inhibitors are generally safe, they require patient education and monitoring:
Routine Monitoring:
-
Kidney function (eGFR, creatinine)
-
Electrolytes
-
Blood pressure and hydration status
Sick Day Guidance:
Patients should temporarily stop SGLT-2 inhibitors during illness, dehydration, or fasting (e.g., vomiting, diarrhea, fever, or surgery). This helps reduce the small risk of rare complications like euglycemic diabetic ketoacidosis.
“SADMANS” Rule: Medications to pause during acute illness:
-
SGLT-2 inhibitors
-
ACE inhibitors
-
Diuretics
-
Metformin
-
ARBs
-
NSAIDs
-
Sulfonylureas
Final Thoughts
At Connecticut Kidney and Hypertension Specialists, we are proud to offer cutting-edge, evidence-based care. These medications are changing lives and reshaping the treatment of kidney disease and cardiovascular risk. For more information please review:: https://www.kidney.org/kidney-topics/sglt2-inhibitors
If you or a loved one has CKD or risk factors for progression, we encourage you to speak with your nephrologist or primary care physician about whether SGLT-2 therapy might be right for you. Contact us today to schedule an appointment and learn more about protecting your kidneys for the long term.
